The Inflammatory Reflex: How Your Vagus Nerve Controls Chronic Inflammation
The groundbreaking discovery that could eliminate chronic disease for millions
Chronic inflammation is the silent killer behind most modern diseases. Heart disease, diabetes, arthritis, Alzheimer's, and even depression—all share a common root: unchecked inflammatory processes that rage through the body, damaging tissues and disrupting normal function.
For decades, the medical approach to inflammation has been simple: suppress it with drugs. But what if there was a better way? What if your body already had a built-in system for regulating inflammation, and all it needed was the right activation?
Dr. Kevin Tracey, a neurosurgeon at the Feinstein Institutes, made a discovery that changed everything. He found that the vagus nerve—the longest cranial nerve in your body—acts as a master regulator of inflammation. This discovery, called the inflammatory reflex, could revolutionize how we treat chronic disease.
The Inflammation Epidemic
Chronic inflammation isn't just a medical concept—it's a worldwide health crisis. More than half of all deaths globally are linked to inflammatory conditions. These include:
- Cardiovascular disease (heart attacks, strokes)
- Type 2 diabetes and metabolic syndrome
- Autoimmune disorders (rheumatoid arthritis, lupus, Crohn's disease)
- Neurodegenerative diseases (Alzheimer's, Parkinson's)
- Certain cancers
- Depression and anxiety disorders
The current treatment approach relies heavily on anti-inflammatory medications. While these drugs can be lifesaving, they come with significant drawbacks:
- Side effects ranging from stomach ulcers to increased infection risk
- High costs (biologics can cost tens of thousands annually)
- Limited effectiveness (only 40-50% of patients respond well)
- Need for continuous use (symptoms return when stopped)
The Accidental Discovery
Dr. Kevin Tracey wasn't looking for an inflammation cure. He was studying the brain's response to injury when he noticed something strange: stimulating the vagus nerve seemed to reduce inflammatory responses throughout the body.
This observation led to years of research that revealed the inflammatory reflex—a neural circuit that uses the vagus nerve to monitor and control inflammation.
"It is like stepping on the brakes in your car. You can slow down the amount of inflammation." — Dr. Kevin Tracey
How the Inflammatory Reflex Works
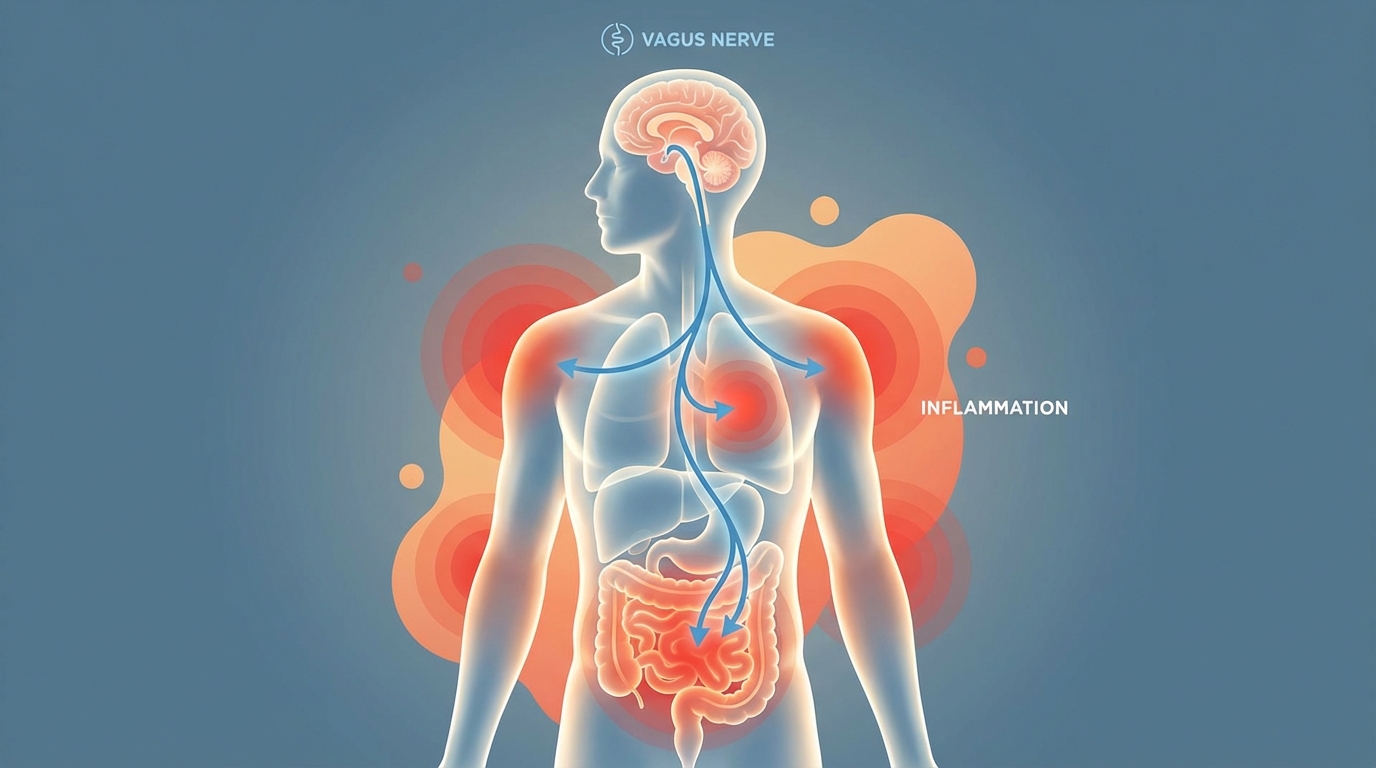
The inflammatory reflex is a negative feedback loop that operates like a neural thermostat for inflammation:
- Detection: The vagus nerve constantly monitors inflammation levels throughout the body via specialized receptors
- Signaling: When inflammation rises, signals travel up the vagus nerve to the brainstem's nucleus tractus solitarius
- Response: The brain sends signals back down the vagus nerve to the spleen via the splenic nerve
- Suppression: The spleen releases acetylcholine, which binds to receptors on immune cells and shuts down inflammatory cytokine production
The key inflammatory cytokines suppressed by this reflex include TNF-alpha, IL-6, and IL-1—the same molecules targeted by expensive biologic drugs like Humira and Enbrel. But instead of using pharmaceuticals to block these molecules, the inflammatory reflex turns off their production at the source.
Bioelectronic Medicine: A New Field
Dr. Tracey's discovery gave birth to an entirely new medical field: bioelectronic medicine. This approach uses devices rather than drugs to treat disease by modulating the body's own neural pathways.
The premise is revolutionary: instead of flooding the body with chemicals that have systemic effects and side effects, bioelectronic medicine precisely stimulates specific nerves to trigger healing responses.
Vagus Nerve Stimulation for Inflammation
Research has shown that artificially stimulating the vagus nerve can activate the inflammatory reflex, reducing inflammation in conditions including:
- Rheumatoid arthritis: Reduced joint swelling and pain
- Inflammatory bowel disease: Decreased gut inflammation
- Sepsis: Better outcomes in life-threatening infections
- Metabolic syndrome: Improved insulin sensitivity
- Post-surgical inflammation: Faster healing
From Surgical to Non-Invasive
Early vagus nerve stimulation for inflammation required surgical implantation of a device. While effective, this limited adoption. But new technologies are changing the landscape:
Transcutaneous VNS
Electrical stimulation through the skin, typically at the ear, can activate the vagus nerve without surgery. Studies show this reduces inflammatory markers and improves symptoms in various conditions.
Focused Ultrasound
Ultrasound waves can penetrate tissue and stimulate the vagus nerve mechanically rather than electrically. Research published in the Journal of Neural Engineering (2022) demonstrated that low-intensity focused ultrasound of the vagus nerve produces measurable autonomic modulation.
Natural Methods
Breathing exercises, cold exposure, meditation, and other practices can increase vagal tone and enhance the body's natural inflammatory reflex. While less potent than device-based stimulation, these approaches are accessible to everyone and can be practiced daily.
The Drug-Free Alternative
For the millions suffering from chronic inflammatory conditions, vagus nerve stimulation offers a radically different approach:
Instead of taking expensive medications with side effects, patients could use vagus nerve stimulation to activate their body's natural anti-inflammatory systems. This isn't science fiction—it's already happening in clinical trials and specialized treatment centers.
Bottom Line
The inflammatory reflex represents one of the most important discoveries in modern medicine. It reveals that inflammation isn't just a biochemical process—it's a neural process that can be modulated through the vagus nerve.
For the millions suffering from chronic inflammatory diseases, this offers hope for treatments that work with the body's natural systems rather than against them. Whether through implanted devices, non-invasive stimulation, or natural practices that enhance vagal tone, we now have tools to address the root cause of inflammation.
The future of medicine may not be in better drugs, but in better understanding and activation of the body's own healing systems. The vagus nerve and the inflammatory reflex are leading the way.