The Vagus Nerve: Your Brain's Secret Weapon Against Depression and Anxiety
The emerging frontier in mental health treatment when medications fail
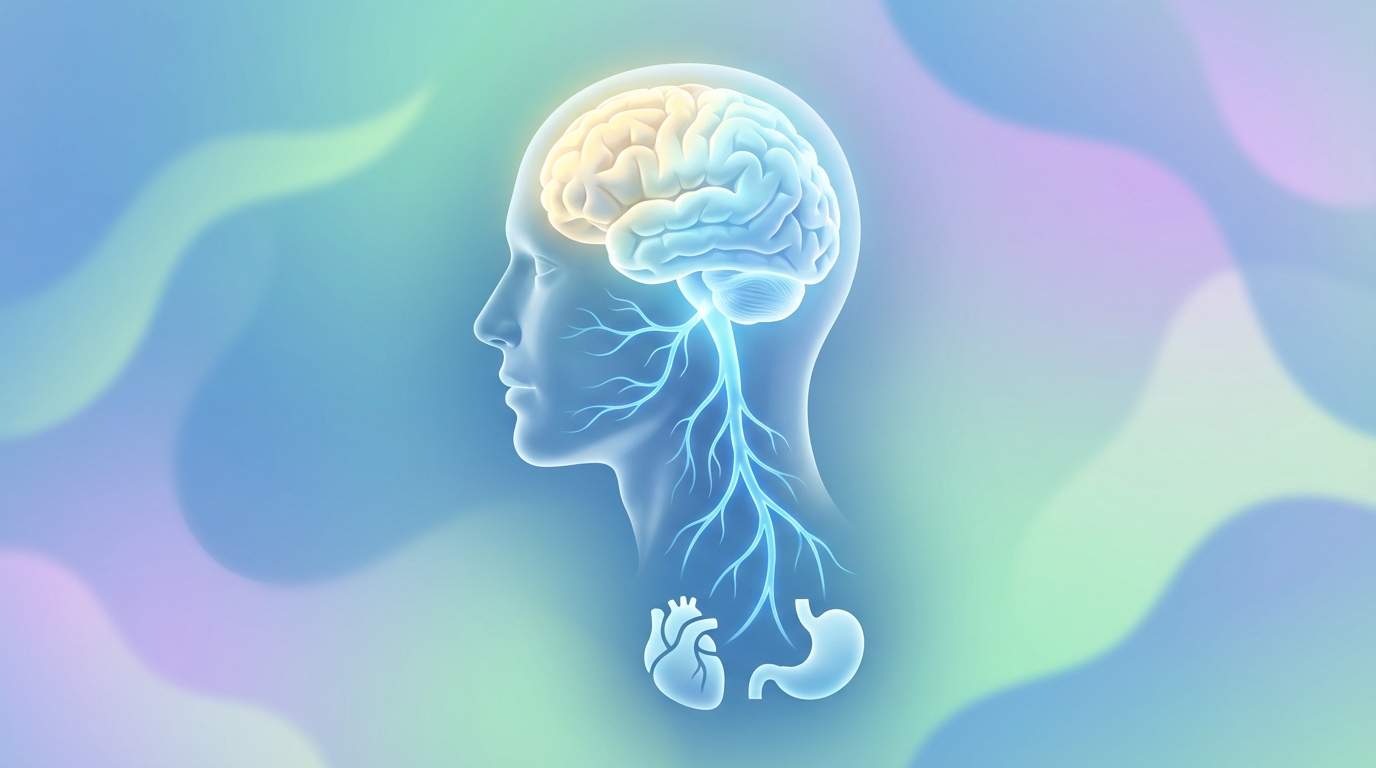
The vagus nerve is emerging as one of the most promising new frontiers in mental health treatment—a neural superhighway that carries signals between your brain and body, with the power to ease depression, calm anxiety, and restore emotional balance when medications fail.
What Is the Vagus Nerve?
The vagus nerve is the longest and most complex of the 12 cranial nerves, earning its name from the Latin word vagary, meaning "wandering." This neural vine extends from the brainstem down through the neck, chest, and abdomen, creating roots in nearly every major organ while sending shoots throughout the brain.
- 80% afferent fibers carry sensory information TO the brain from the body
- 20% efferent fibers send regulatory signals FROM the brain to the body
This unique architecture means the vagus nerve doesn't just receive reports from your organs—it actively participates in shaping how you think, feel, and respond to stress.
The Accidental Discovery That Changed Psychiatry
The connection between vagus nerve stimulation and mental health was discovered almost by accident. In 1997, the FDA approved implantable vagus nerve stimulation (VNS) for treatment-resistant epilepsy. During clinical trials, researchers noticed something unexpected: patients consistently reported improvements in their mood, even when their seizures continued.
When researchers offered to remove the devices from patients whose epilepsy hadn't improved, many refused. "No, leave it in," they said. "It makes me feel good."
This observation prompted a new line of research. By 2005, the FDA approved VNS for treatment-resistant depression—the first new treatment for depression in decades that worked through a completely different mechanism than traditional antidepressants.
How Vagus Nerve Stimulation Affects the Brain
Vagus nerve stimulation works by sending gentle electrical signals up the afferent fibers to the brainstem's nucleus tractus solitarius. From there, signals cascade to multiple brain regions involved in mood regulation:
The Amygdala
The brain's fear and anxiety center receives direct input from the vagus nerve. Stimulation helps reduce hyperactivity in this region, calming the fight-or-flight response that drives anxiety disorders.
The Hypothalamus
This region controls stress hormone release, including cortisol. VNS helps normalize the hypothalamic-pituitary-adrenal (HPA) axis, reducing the physiological stress response that contributes to depression.
The Ventral Tegmental Area
The brain's reward and pleasure center receives modulation via vagus nerve pathways. Stimulation can help restore the dopamine signaling often impaired in depression, bringing back the capacity for joy and motivation.
The Prefrontal Cortex
Higher cognitive functions including emotional regulation and decision-making improve with enhanced vagal tone, supporting better mood management and resilience.
The Depression Connection: When Antidepressants Aren't Enough
Treatment-resistant depression affects approximately 30% of people diagnosed with major depressive disorder. These individuals try multiple antidepressant medications without finding relief, leaving them in a treatment desert with few options.
Vagus nerve stimulation offers a lifeline. Clinical studies show that while VNS doesn't work as quickly as antidepressants—it can take months rather than weeks to show full effects—it produces durable, long-lasting improvements in mood for many patients who had exhausted other options.
Beyond Depression: Vagus Nerve and Anxiety Disorders
The vagus nerve's role in calming the amygdala makes it a natural target for anxiety treatment. Research shows:
- Generalized anxiety disorder patients show reduced symptoms with VNS treatment
- Panic disorder severity decreases as vagal tone improves
- PTSD symptoms including hypervigilance and emotional reactivity respond to vagus nerve modulation
- Social anxiety improves as the threat-detection systems calibrate more accurately
Unlike benzodiazepines and other anti-anxiety medications, vagus nerve stimulation doesn't cause sedation, dependence, or cognitive impairment. It works by strengthening the body's natural calming systems rather than overriding them.
The Inflammation-Depression Link
One of the most exciting discoveries in neuroscience is the connection between inflammation and depression. Researchers now understand that inflammatory cytokines—chemical messengers of the immune system—can cross the blood-brain barrier and trigger depressive symptoms.
The vagus nerve plays a central role in this story through the inflammatory reflex:
- The vagus nerve constantly monitors inflammation levels throughout the body
- When inflammation rises, vagal signals travel to the spleen via the splenic nerve
- The spleen releases acetylcholine, which binds to receptors on immune cells
- This signal reduces production of pro-inflammatory cytokines including TNF-alpha, IL-6, and IL-1
By stimulating the vagus nerve, we can activate this natural anti-inflammatory pathway—potentially addressing the biological roots of inflammation-driven depression.
Non-Invasive Options: Stimulating Without Surgery
While FDA-approved VNS requires surgical implantation of a device, researchers have developed non-invasive alternatives that make vagus nerve modulation accessible to everyone:
Transcutaneous Vagus Nerve Stimulation (tVNS)
Devices that deliver gentle electrical pulses through the skin—typically at the ear or neck—can activate the vagus nerve without surgery. Multiple studies show tVNS reduces acute stress, improves anxiety symptoms, and enhances emotional regulation.
Cold Exposure
Cold water immersion on the face triggers the mammalian dive reflex, a powerful vagal activation response. Even brief cold exposure—30 seconds of cold water on the face or a cold shower finish—can increase parasympathetic tone and reduce anxiety.
Deep Breathing Protocols
Slow diaphragmatic breathing at approximately 6 breaths per minute creates resonance in the cardiovascular system that maximally stimulates the vagus nerve. This "resonance frequency breathing" has been shown to reduce anxiety and improve heart rate variability.
Humming and Chanting
The vagus nerve passes through the larynx and vocal cords. Vocalization—including humming, chanting, singing, and even gargling—activates these vagal pathways, providing an accessible way to boost vagal tone throughout the day.
The Science of Vagal Tone
Vagal tone refers to the activity level of the vagus nerve, measured primarily through heart rate variability (HRV)—the variation in time between heartbeats. Higher HRV indicates stronger vagal tone and better autonomic nervous system balance.
The encouraging news: vagal tone is not fixed. Through consistent practice of vagus-activating techniques, you can strengthen this neural pathway and enhance your mental health resilience.
Bottom Line
The vagus nerve represents a paradigm shift in mental health treatment—moving from chemical interventions that flood the brain to neuromodulation techniques that help the brain heal itself. Whether through FDA-approved implanted devices or simple daily practices like cold exposure and deep breathing, vagus nerve stimulation offers hope for the millions struggling with treatment-resistant depression and anxiety.