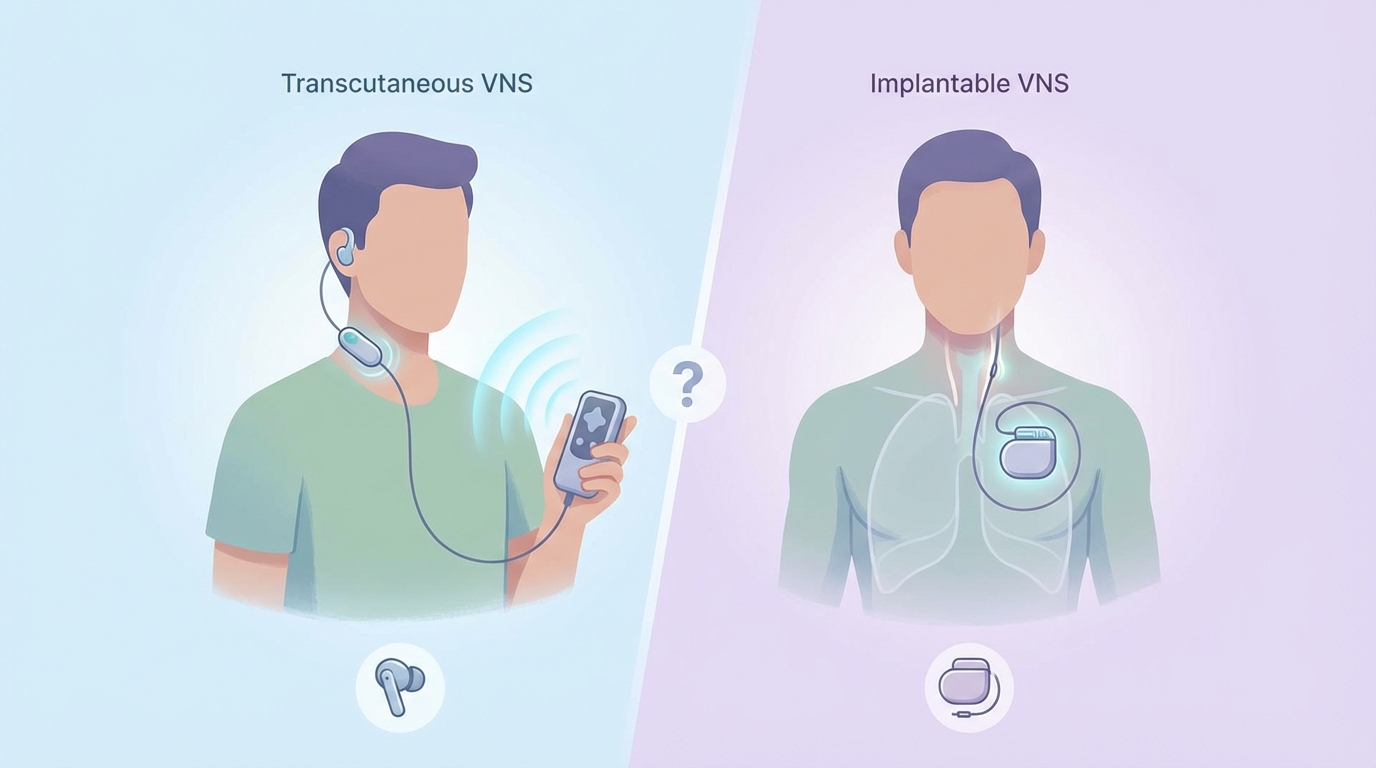
Transcutaneous vs. Implantable VNS: Which Is Right for You?
A complete comparison of invasive and non-invasive vagus nerve stimulation options
The Evolution of Vagus Nerve Stimulation
Vagus Nerve Stimulation has transformed from an experimental treatment to an FDA-approved therapy for epilepsy and depression. But not all VNS is created equal. The field has evolved from surgical implants to non-invasive alternatives that offer similar benefits without the risks and costs of surgery.
Understanding the differences between implantable VNS (iVNS) and transcutaneous VNS (tVNS) is crucial for making informed decisions about your health. This guide breaks down everything you need to know.
Implantable VNS: The Original Approach
How It Works
Implantable VNS requires surgical placement of a pulse generator (similar to a pacemaker) under the skin in the chest, with a lead wire wrapped around the cervical vagus nerve in the neck. The device delivers electrical impulses at programmed intervals.
Pros of Implantable VNS
- Proven efficacy: 25+ years of clinical data for epilepsy and depression
- FDA approved: Covered by insurance for approved indications
- Continuous stimulation: 24/7 therapy without user intervention
- Precise targeting: Direct nerve contact for consistent stimulation
- Magnet activation: Patients can trigger extra stimulation when needed
Cons of Implantable VNS
- Surgical risks: Infection, bleeding, nerve damage (1-3% complication rate)
- High cost: 0,000-0,000+ for device and surgery
- Side effects: Hoarseness, coughing, throat pain, sleep apnea
- Battery replacement: Requires surgery every 3-10 years
- Irreversible: Permanent implant (though removable with surgery)
- Limited availability: Only approved for specific conditions
Transcutaneous VNS: The Non-Invasive Revolution
How It Works
Transcutaneous VNS stimulates the vagus nerve through the skin, targeting either the auricular branch (outer ear) or cervical branch (neck). No surgery required — devices use surface electrodes or ultrasound.
Types of tVNS
2. Cervical tVNS: Targets the vagus nerve in the neck using surface electrodes. Requires proper placement but offers stronger stimulation.
3. Ultrasound VNS: Emerging technology using focused ultrasound waves to stimulate the nerve without skin contact. No electrodes needed.
Pros of Transcutaneous VNS
- No surgery: Zero surgical risks or recovery time
- Lower cost: Hundreds to thousands of dollars vs. tens of thousands
- Self-administered: Use at home without medical supervision
- Adjustable: Easy to modify intensity and duration
- No side effects: Minimal to no adverse effects reported
- Reversible: Stop anytime without medical intervention
- Broad applications: Can be used off-label for various conditions
Cons of Transcutaneous VNS
- Emerging evidence: Less long-term data than implanted devices
- Requires active use: Must be applied regularly for benefits
- Variable results: Effectiveness depends on proper placement
- Not FDA approved: Most devices are wellness products, not medical devices
- Weaker stimulation: Surface delivery vs. direct nerve contact
Head-to-Head Comparison
| Factor | Implantable VNS | Transcutaneous VNS |
|---|---|---|
| Cost | $20,000-$40,000+ | $200-$2,000 |
| Surgery Required | Yes | No |
| Recovery Time | 2-4 weeks | None |
| FDA Approved | Yes (epilepsy, depression) | No (wellness category) |
| Insurance Coverage | Yes (for approved uses) | No |
| Clinical Evidence | 25+ years, extensive | 10+ years, growing |
| Side Effects | Common (hoarseness, cough) | Rare (mild skin irritation) |
| Maintenance | Battery replacement surgery | Device replacement/recharge |
| Control | Programmed by physician | User-controlled |
Which Should You Choose?
- You have treatment-resistant epilepsy or depression
- You have tried multiple medications without success
- You want continuous, automated stimulation
- You have insurance coverage for the procedure
- You are comfortable with surgical risks
- You want to avoid surgery
- You have anxiety, stress, or mild-moderate depression
- You want to improve sleep, focus, or HRV
- You prefer a lower-cost option
- You want to try VNS before committing to surgery
- You are seeking general wellness benefits
The Emerging Winner: Ultrasound VNS
While both implanted and surface-electrode tVNS have their places, ultrasound VNS represents the best of both worlds:
- Non-invasive like tVNS
- Precise targeting like implanted devices
- No skin irritation from electrodes
- Deeper tissue penetration for cervical vagus access
- Emerging clinical evidence for anxiety, inflammation, and pain
The Bottom Line
For severe, treatment-resistant conditions, implantable VNS remains the gold standard with proven long-term results. But for the vast majority of people seeking better mental health, reduced stress, improved sleep, or general wellness, transcutaneous VNS offers an accessible, affordable, and risk-free alternative.
The field is evolving rapidly. As research accumulates, the line between invasive and non-invasive VNS continues to blur. The future likely holds FDA-approved non-invasive devices that combine the efficacy of implants with the safety of surface stimulation.
The best VNS device is the one you will actually use. For many, that means starting with non-invasive options and only considering surgery if absolutely necessary.
- Implantable VNS is proven but requires surgery and costs 0,000+
- Transcutaneous VNS is accessible, affordable, and risk-free
- Implanted devices are FDA-approved for epilepsy and depression
- tVNS is ideal for wellness, anxiety, and general health optimization
- Ultrasound VNS may offer the best of both approaches